The CDC has released disturbing information about a case of monkeypox in a baby less than two months old. The infant got sick with the virus after he or she “shared a bed with” two “caregivers” for six weeks, including an infected man who had engaged in risky behavior.

According to the newly-public report, the baby was brought to a Florida hospital Emergency Room with a rash on his or her arms, legs, and trunk. Doctors tested the child for bacterial infections, chicken pox, herpes, and HIV, but results were negative. Two days later the baby was admitted to the hospital with “papulovesicular lesions over the body.” At that time, the infant tested positive for monkeypox.
The lesions subsequently spread to the back, soles of feet, face, and eyelid and became pustular over the first few days of [hospital] admission.
Centers for Disease Control (CDC) report on youngest Florida patient to be diagnosed with monkeypox
According to CDC, “the infant [had been] cared for by four caregivers” referred to as Caregivers A, B, C, and D. The report implied it was “Caregiver B” who likely transmitted monkeypox to the baby because that man “reported activities that placed him at high risk for monkeypox exposure during the 2 months preceding the infant’s illness,” and was also subsequently diagnosed with monkeypox. Monkeypox is typically spread through the act of sex or intimate contact between men.

CDC says Caregiver B reported that he had blood in his urine and a rash within three weeks prior to the baby becoming sick. A day before the baby showed symptoms, Caregiver B “moved to another state…sought medical care…received a positive [monkeypox] test” and was “lost to follow-up.”
CDC says the infected man had “had daily close contact” with the baby for six weeks prior to the infant’s rash outbreak. He and another caregiver “shared a bed for the 6 weeks preceding the infant’s symptom onset” and all four household members “held the infant with close skin-to-skin contact.”
After hospital treatment, the baby recovered. The CDC report did not say whether child welfare authorities were notified, or whether there was any investigation into the health and safety circumstances of the baby.
Read the CDC at this link and pasted below.
Monkeypox in a Young Infant — Florida, 2022
In August 2022, the Florida Department of Health (FDOH) was notified of a suspected case of monkeypox in an infant aged <2 months who was admitted to a Florida hospital with a rash and cellulitis. This case report highlights findings from the related epidemiologic investigation and describes the public health actions taken. This activity was reviewed by CDC and was conducted consistent with applicable federal law and CDC policy.* This is the youngest patient with confirmed monkeypox infection in Florida to date.
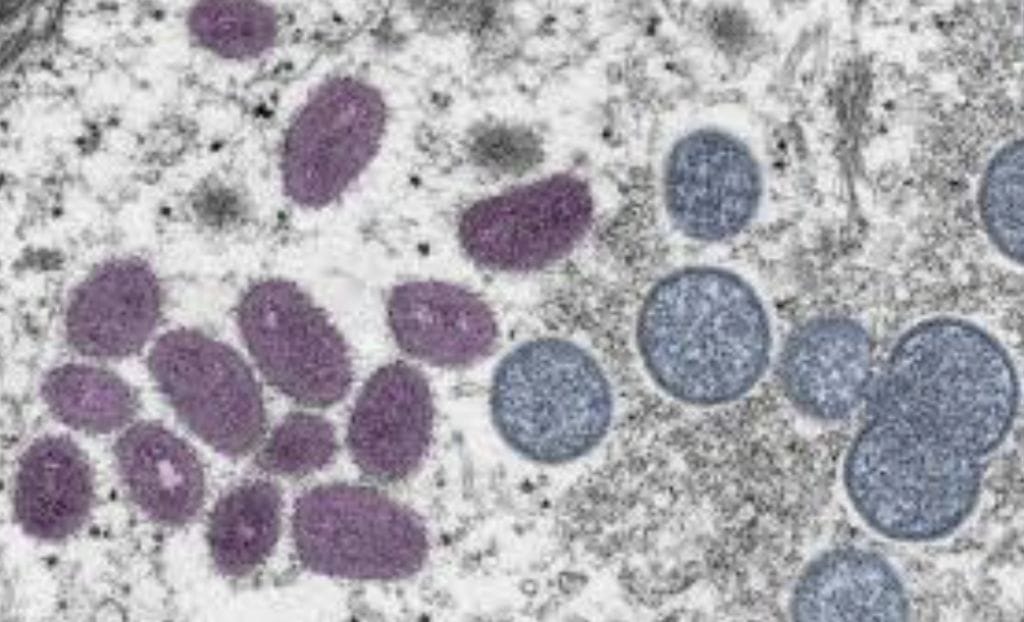
The infant was initially evaluated in an emergency department (ED) for a raised erythematous rash on the arms, legs, and trunk which had been present for 5 days. A rash swab was collected for bacterial culture and yielded a negative test result. Varicella, herpes simplex virus, and HIV testing were also negative. The patient returned to the ED 2 days later, at which time the rash had progressed to include numerous, diffusely scattered papulovesicular lesions over the body, many with central umbilication. The infant was admitted to the hospital with a diagnosis of molluscum contagiosum and started on intravenous antibiotics for secondary bacterial cellulitis associated with having scratched a lesion on the arm. The lesions subsequently spread to the back, soles of feet, face, and eyelid and became pustular over the first few days of admission. Swabs from forehead and back lesions tested positive for Orthopoxvirus DNA and Clade II Monkeypox virus DNA by polymerase chain reaction 10 days after rash onset (Figure). Results were confirmed by the Florida public health laboratory and CDC.† FDOH and hospital clinicians consulted with CDC regarding treatment options. The infant was treated with oral tecovirimat and Vaccinia Immune Globulin Intravenous (1). Prophylactic trifluridine§ drops were administered to prevent ophthalmic complications from the eyelid lesion. The infant remained afebrile and stable throughout the course of illness, tolerated the treatments well, and fully recovered.
The infant had no history of travel, no history of acute infections in the 3 weeks preceding rash onset, no known immunocompromising conditions, did not attend a child care facility, and had no caregivers outside the home. Within the home, the infant was cared for by four caregivers. Caregiver A acted as the main guardian throughout the infant’s hospital stay and had prolonged exposure with skin-to-skin contact. Caregiver B reported activities that placed him at high risk for monkeypox exposure during the 2 months preceding the infant’s illness (2). Caregiver B reported hematuria and fever, followed by a rash within the 3 weeks before the infant’s symptom onset. One day before the infant became symptomatic, caregiver B moved to another state and sought medical care for his symptoms. He received a positive Orthopoxvirus DNA test result 2 days after the infant’s positive test result, after which, he was lost to follow-up. The infant had daily close contact with caregiver B in the home for 6 weeks before rash onset. Possible routes of transmission included shared bed linens and skin-to-skin contact through holding and daily care activities. Investigation identified three other household family members with household exposures to both the infant and caregiver B. Caregiver B, caregiver C, and the infant shared a bed for the 6 weeks preceding the infant’s symptom onset. All household members (caregivers A, B, C, and D) held the infant with close skin-to-skin contact. Caregivers A, C, and D received postexposure prophylaxis with JYNNEOS vaccine and remained asymptomatic at 22 days after the infant’s symptom onset (2,3). Caregiver A had also received smallpox vaccination during childhood.
To date, 27 confirmed cases of monkeypox in pediatric patients aged 0–15 years have been reported in the United States during the 2022 outbreak (4). Clinical presentations in children with monkeypox have been similar to those in adults, although children might have a higher risk for severe disease (5). Timely laboratory identification and thorough epidemiologic investigation are critical for effective public health response to monkeypox infection. In this case, contact tracing and postexposure prophylaxis vaccination of close contacts of the affected infant might have prevented further transmission to household members (3). Clinicians should consider monkeypox infection as a differential diagnosis in pediatric patients with pustular or vesicular rashes and be aware of the possibility for household transmission to pediatric patients, particularly if the children meet epidemiologic exposure criteria for diagnosis of monkeypox (6).


